We are developing injectable hydrogels for better engraftment of cardiac and skeletal muscle stem cells in various muscle pathologies, including myocardial infarction, traumatic injuries, and muscular dystrophy. In these applications, our cell-encapsulating biodegradable hydrogels have been tested pre-clinically as cell carriers, effectively localizing the cell grafts, providing protection against inflammation and facilitating controlled integration with the host tissue
Cardiac cell therapy
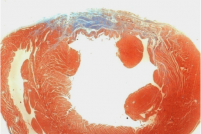
In situ delivery of hydrogel biomaterials together with cell grafts promises to help overcome some of the enduring challenges in the field of cardiac cell therapy. For example, injectable biodegradable materials used as cardiac cell carriers aim to overcome the problems associated with poor cell engraftment into a myocardial infarction (MI) by providing both temporary protection for the graft while promoting better long-term cell survival. Injectable biomaterials that polymerize in situ and encapsulate cells can potentially protect the cell graft from inflammation, thus localizing and amplifying the beneficial effects of the injected cells in the harsh, ischemic environment of a muscle injury. Premised on these concepts, we have been working on myocardial repair strategies using in situ polymerizable semi-synthetic hydrogels in combination with both stem cells and allogeneic cell therapies. Our approach is specifically based on the delivery of the exogenous cardiomyocytes together with a biodegradable hydrogel made from PEG-fibrinogen (PF) matrix. First, we optimize the PF hydrogels for in vitro 3D culture with neonatal rat ventricular cardiomyocytes (NRVCMs) or human embryonic stem cell derived cardiomyocytes (hESC-CMs). Ultimately we extend these in vitro results to an in vivo setting by evaluating the feasibility of using the optimized PF matrix to locally deliver the cells in a rat ischemic heart model of MI.
Skeletal muscle cell therapy
We have been working on a combined biomaterials and cell therapy approaches to regenerate skeletal muscle for treating a variety of skeletal muscle diseases characterized by severe loss of function. We focus our investigations on cell-compatible hydrogel biomaterials that, when used as cell carrier for myogenesis, are capable of promoting myogenic cell differentiation in vivo. This strategy entails bioactivity from the biomaterials that also favors angiogenesis and innervation to occur during muscle fiber formation and maturation in situ. Much of our research to date has been centered on mouse mesoangioblasts (Mabs) in PEG-fibrinogen (PF). The Mabs are genetically engineered to express Placenta-derived Growth Factor (PlGF), to attract host vessels and nerves while myotubes begin to form in the implant locale. For example, when PF/Mabs grafts are implanted underneath the skin on the surface of the tibialis anterior (TA), the Mabs form mature and oriented muscle fibres. The normal contractile activity of the underlying muscle provides mechanical stimuli that propagate cell differentiation, and ultimately culminates in an extra muscle that is morphologically and functionally almost indistinguishable from the host tissue. This strategy opens the possibility of in vivo autologous muscle generation for a large number of pathological conditions, including localized muscular dystrophies, post-trauma or post-surgery tissue ablation, and incontinent sphincters.
Relevant Publications
No publications found.